
By Josh Baxt
Voice assistants such as Amazon’s Alexa and Apple’s Siri have tremendous potential to help people manage their health as they age. Using these eye- and hands-free tools, patients could make appointments, confer with clinicians, receive medication reminders and perform other tasks. Unfortunately, current devices have not been designed with older patients, or even healthcare, in mind.
Now, researchers at UC San Diego’s Qualcomm Institute, the Human-centered eXtended Intelligence Research Lab and other programs in UC San Diego’s Computer Science and Engineering Department and Department of Medicine, are taking a hard look at whether older adults are using (or not using) this technology and how it can be improved. Their project is called Voice Assistant for Quality of Life and Healthcare Improvement in Aging Populations, or VOLI, and the voice assistant that resulted is being tested in homes beginning this month as part of a feasibility study.
“Voice assistants have become ubiquitous and could really improve wellbeing for older adults,” said VOLI principal investigator Emilia Farcas, an assistant research scientist at the Qualcomm Institute. “There are many services and products out there, but their adoption is really questionable because you can't just develop something, put it out there and hope it will be used.”
Technological Barriers
Farcas, co-investigator Nadir Weibel, a Computer Science and Engineering professor who heads the Human-centered eXtended Intelligence Research Lab, and colleagues have been assessing the many barriers that reduce effectiveness. In a paper presented at the 23rd International ACM SIGACCESS Conference on Computers and Accessibility (ASSETS'21), the team explored the different issues older people face when using voice assistants.
“We tried to connect to older adults’ real lives,” said Computer Science and Engineering Ph.D. student Chen Chen, first author on the paper. “We wanted to pinpoint their daily life and healthcare management routines – contacting doctors, scheduling appointments, recording their vital signs and submitting them through MyChart (UC San Diego’s electronic health record system) – and we identified some of the problems they are facing.”
The team interviewed 16 people ages 68 to 90, two geriatricians and three nurses to understand how virtual assistants can be useful and where they fall short. They found current devices are poorly designed to manage most healthcare needs.
Tracking medication compliance is just one example. Sometimes patients forget to take their medicines and compound the problem by taking time-sensitive medications whenever they remember, which can lead to bad results. Throughout the study, patients described the functions they wanted.
“I have to weigh myself every day and take my blood pressure and my sugar and keep all that down,” said one study participant. “And my friend said it would be a great thing for me to be able to have Alexa keep that information and then just be able to transfer to MyChart instead of me having that typed all in for the doctors.”
New Designs, New Devices
The VOLI team envisions devices that are more user-friendly and useful to better support older patients. Health-focused voice assistants could prevent emergency room visits and hospitalizations, generally improve quality of life and act as extra sets of eyes and ears for clinicians and concerned family members.
“We need to think about these systems from a more holistic perspective,” said Weibel. “The patient may be the only one actually talking to the device, but we must also consider clinicians and family. What are their needs and how can we support them?”
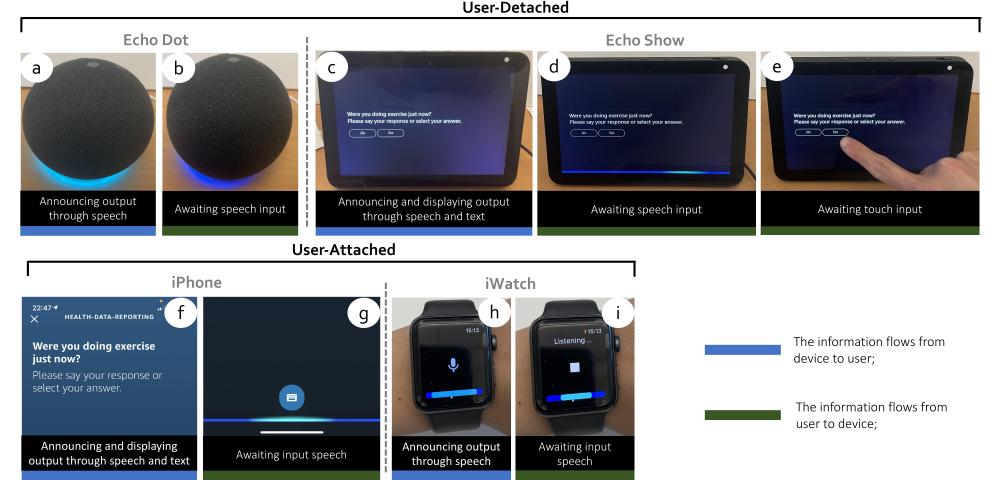
The group is custom designing its own voice assistants and anticipate placing them in households this month. This feasibility study will assess the technology’s effectiveness and provide feedback to continuously refine it. VOLI will initially enroll 10 participants and then scale up to 50. Each participant will receive two devices to test assistant efficacy both with and without a screen.
“This will be an iterative project, during which we test new designs in patients’ homes and see how they work,” said Farcas. “We can then use that information to redesign the devices to make them more effective and give patients, doctors and family members better value.”
VOLI’s interdisciplinary team also includes UC San Diego Department of Medicine co-investigators Alison Moore, the Larry L. Hillblom Chair in Geriatric Medicine and Professor and chief of the Division of Geriatrics and Gerontology, and Michael Hogarth, Professor in the Division of Biomedical Informatics, Director of Biomedical Informatics at the Altman Clinical Translational Science Institute (ACTRI) and Chief Clinical Research Information Officer for UC San Diego Health, as well as Ndapa Nakashole, an assistant professor in the Department of Computer Science and Engineering and a member of the UC San Diego Artificial Intelligence Group.

